RemitData
A real-time, data-rich platform that delivered better patient outcomes
Brief
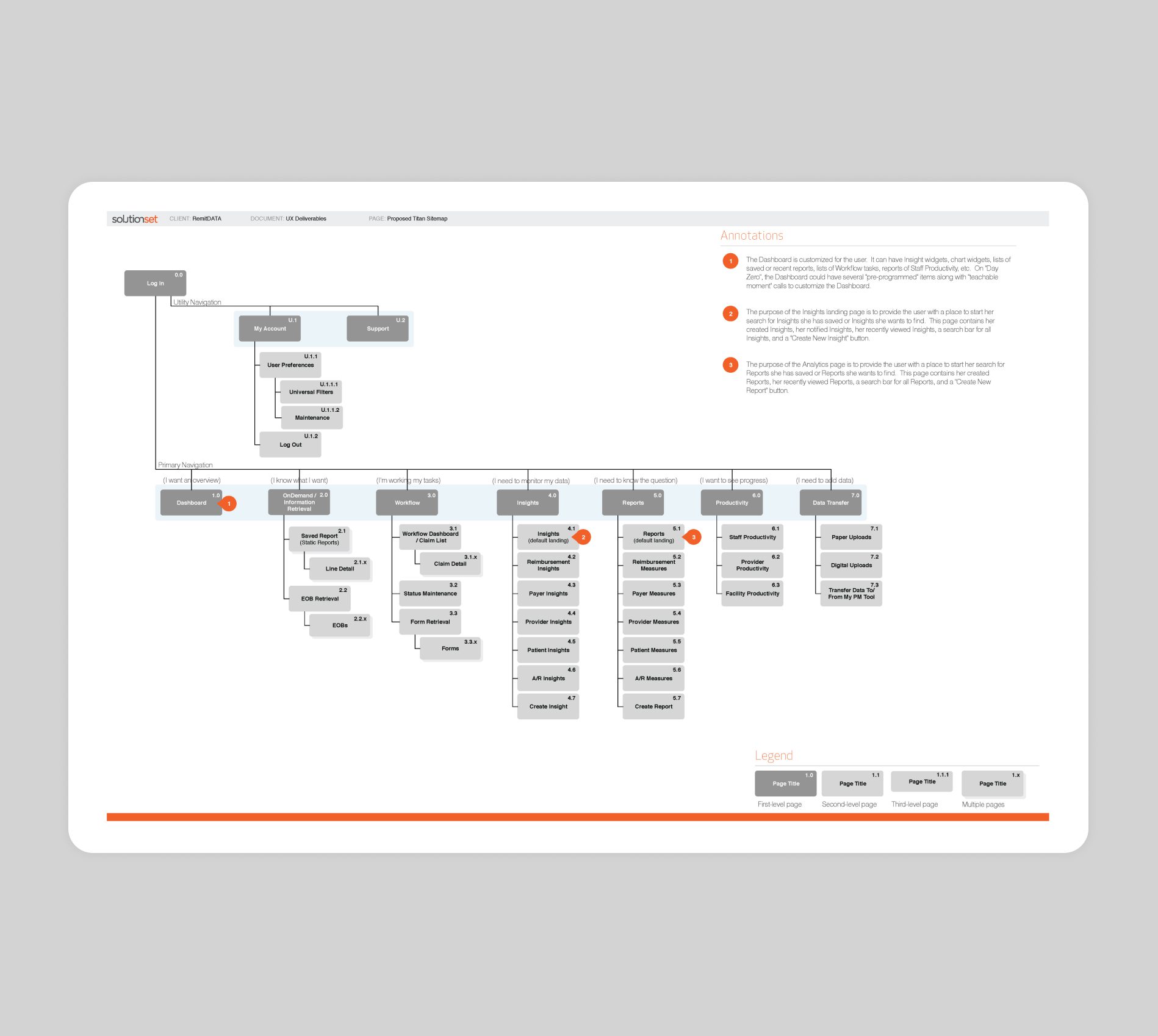
Healthcare providers were challenged with decreasing reimbursement rates, claim denials, increased risk of audits, unending regulatory changes, and improving operational efficiencies to control costs. Performance issues that harm a provider’s bottom line had to be identified and corrected to optimize revenue. RemitData saw these gaps as an opportunity to introduce TITAN, a SaaS application that empowered organizations to spend more time solving problems and less time searching for data.
Details
- Product identity
- Web app
- Built on a proprietary framework
Role
- Digital strategy
- UX and creative direction
Approach
TITAN provided the necessary tools, including transparent comparative data, proactive financial and productivity insights, workflow integration, and utilization monitoring, to enable providers to compete better and thrive in an evolving healthcare landscape.

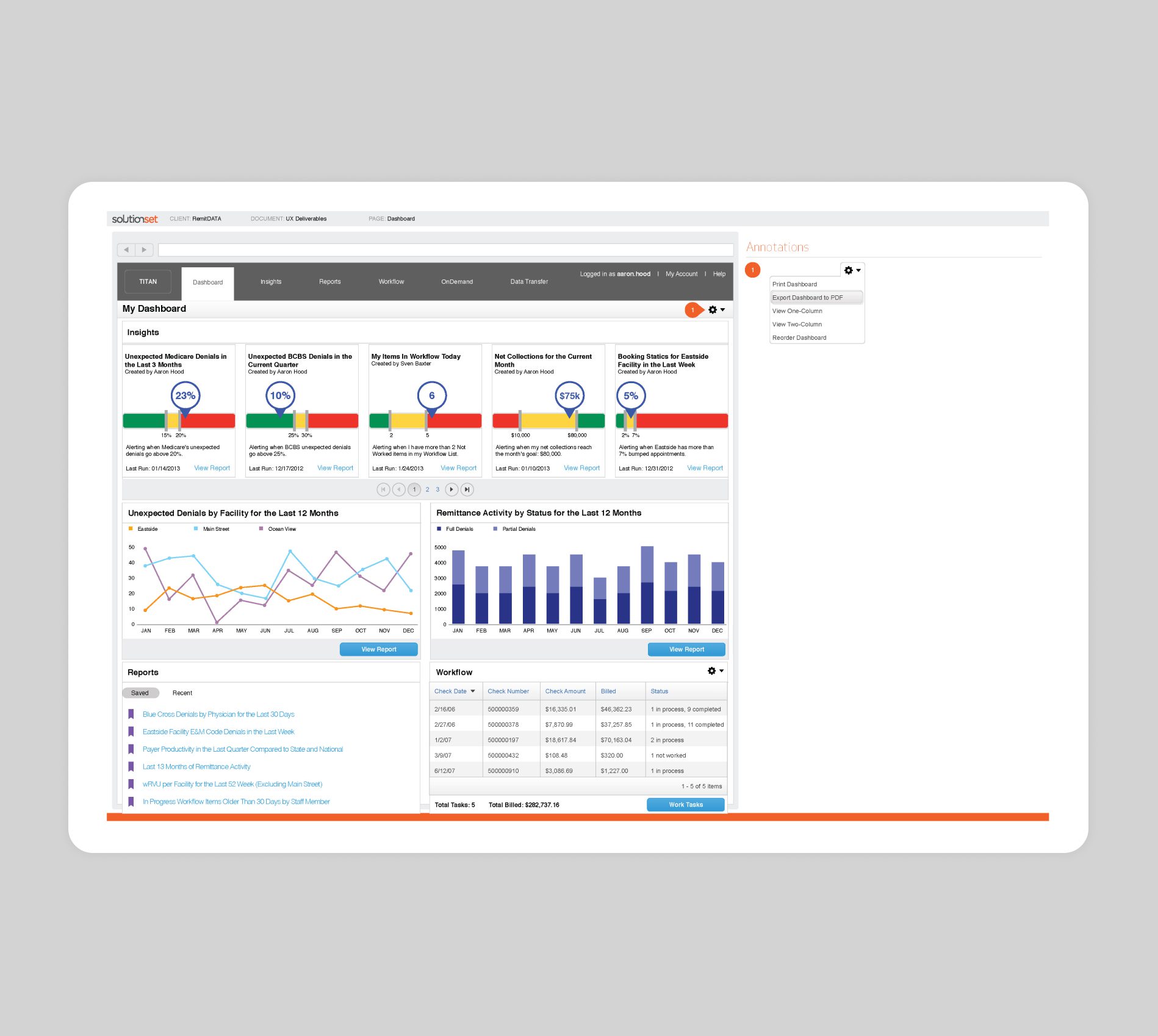
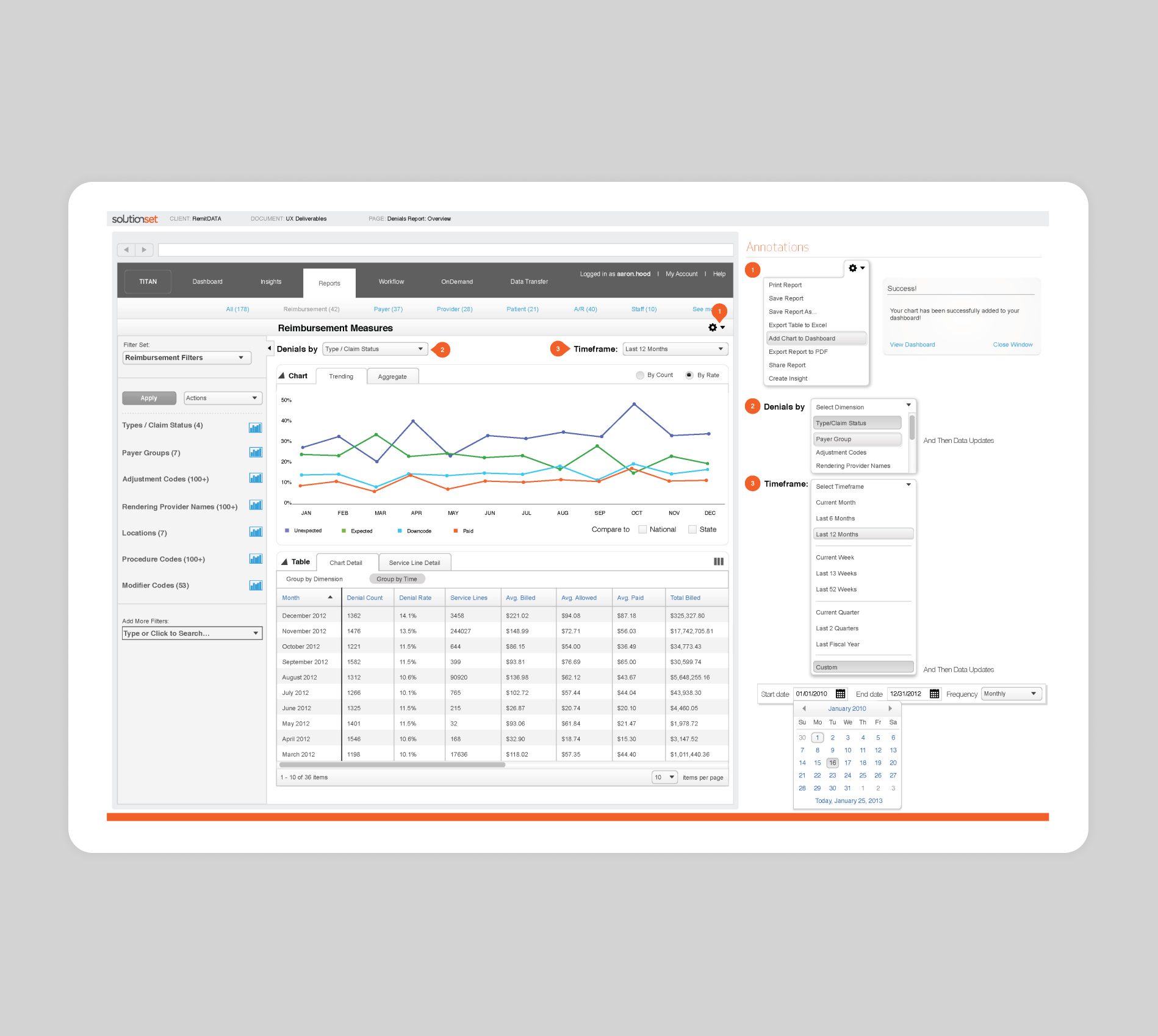
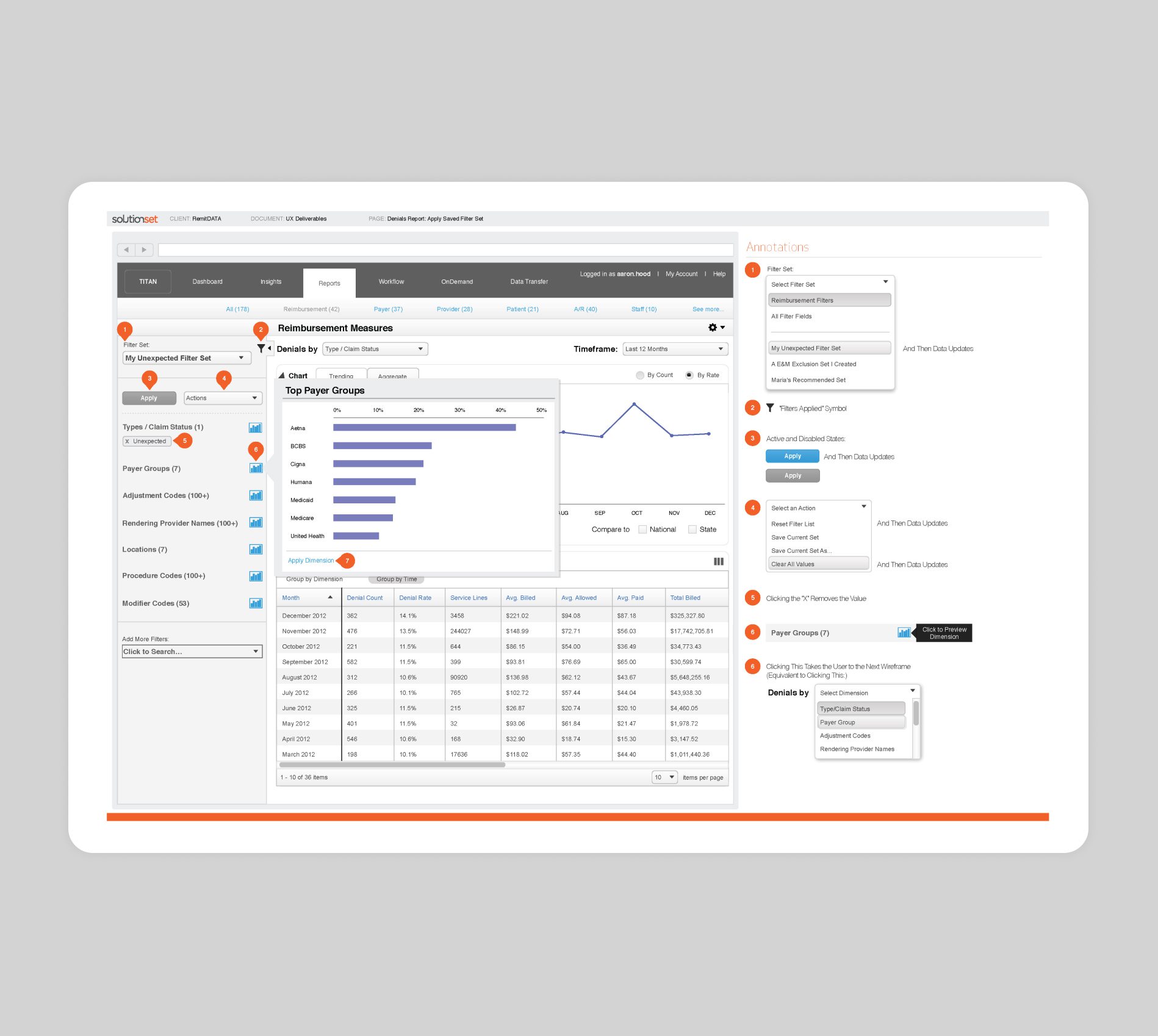
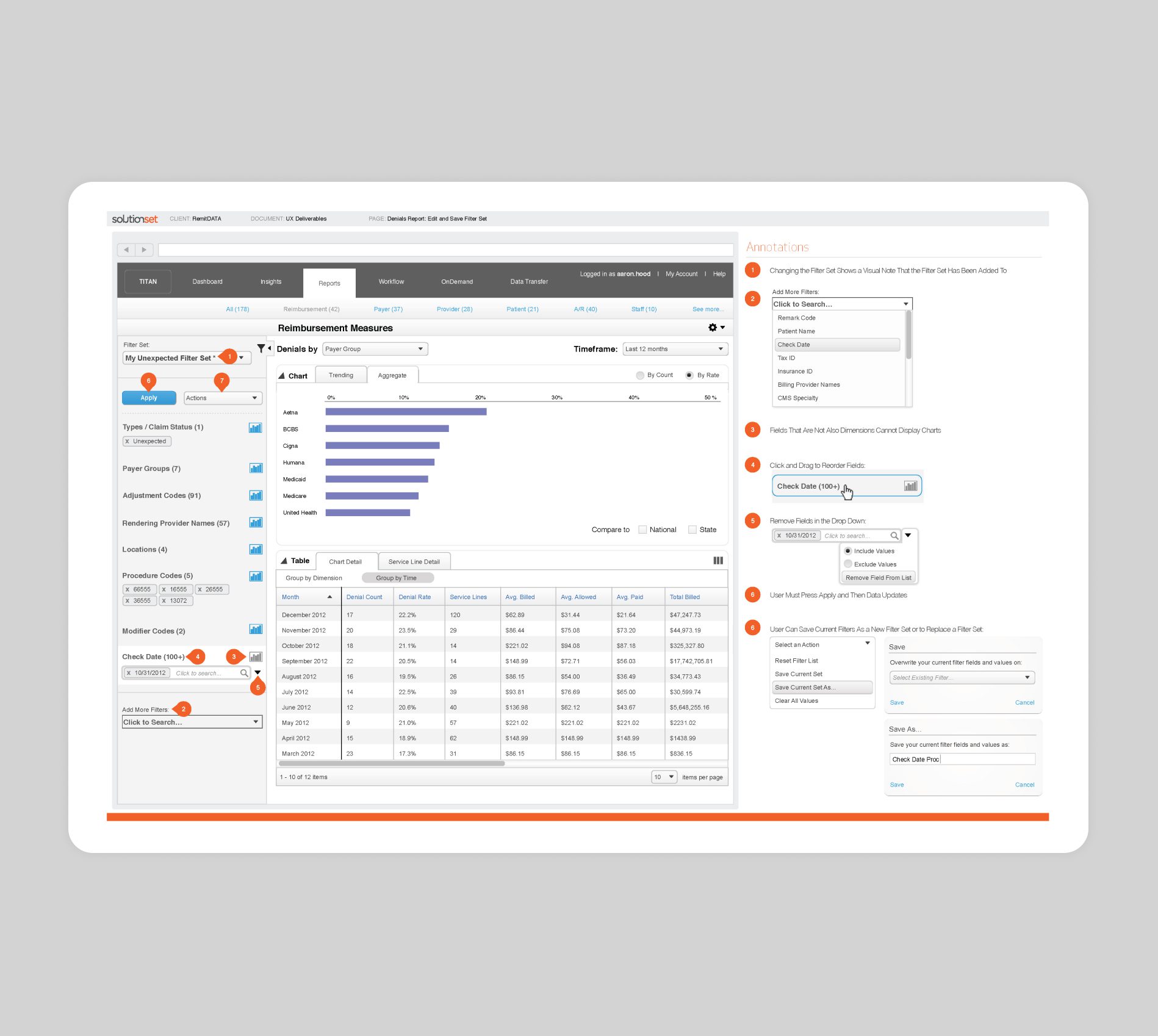
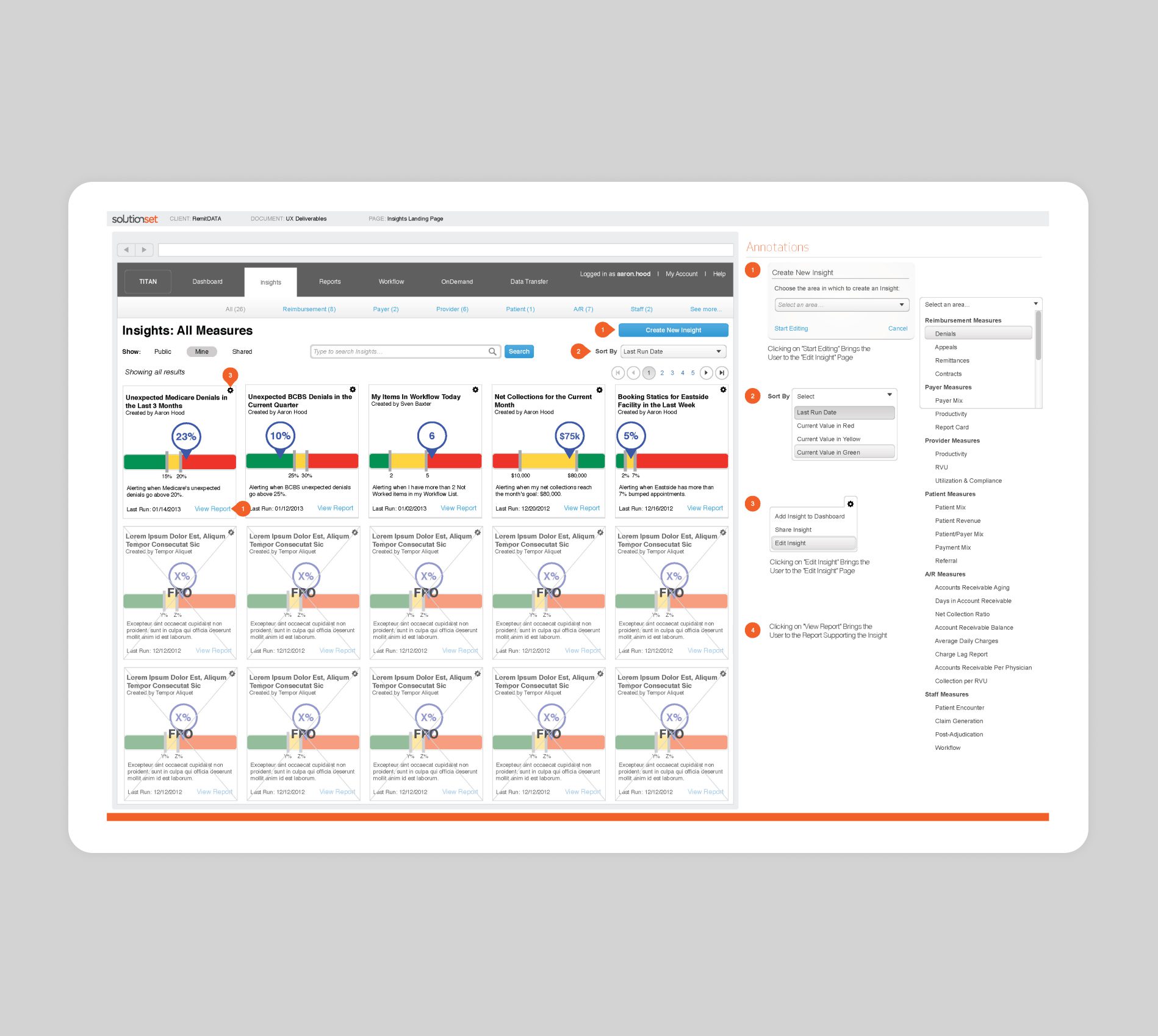
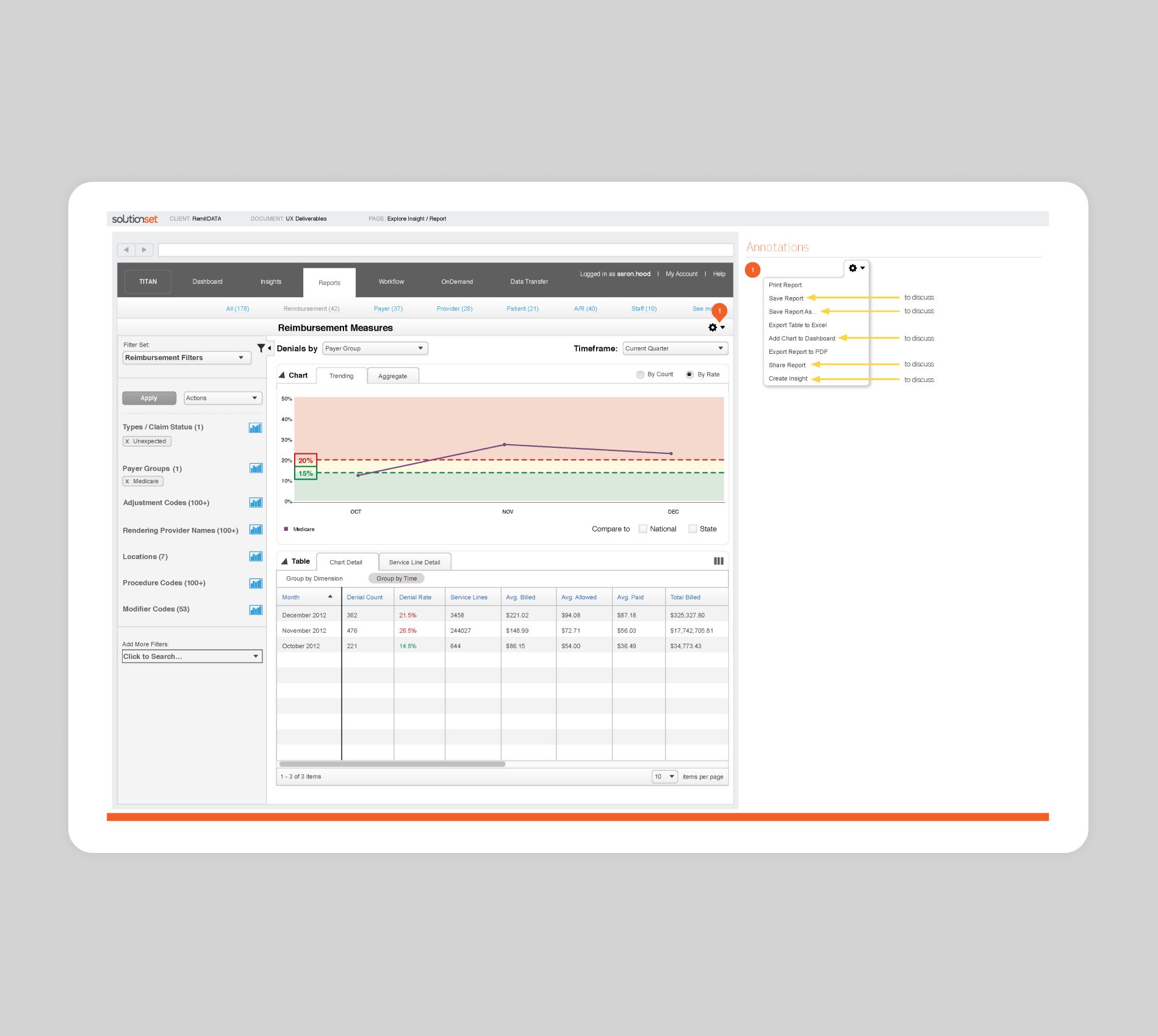
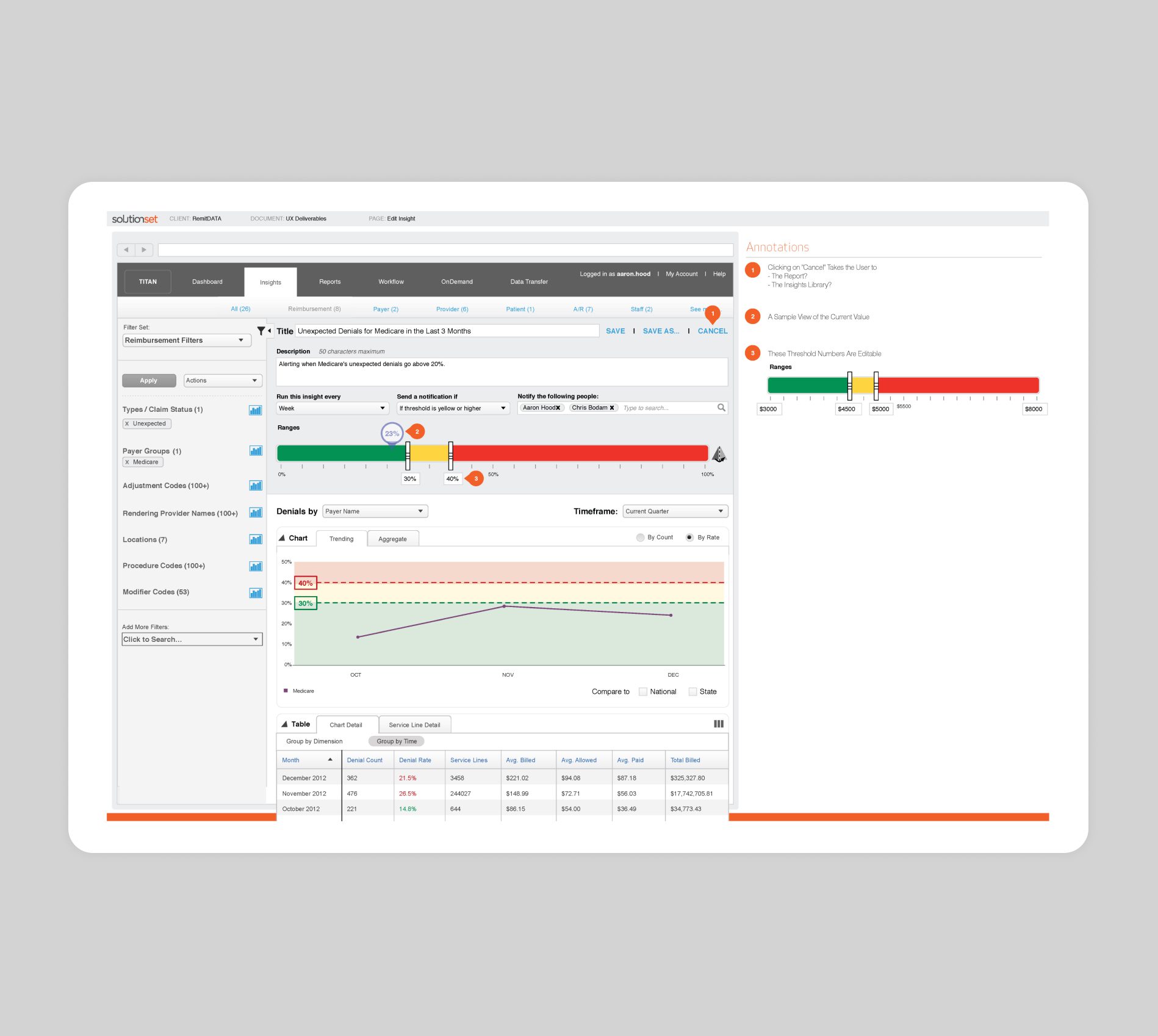
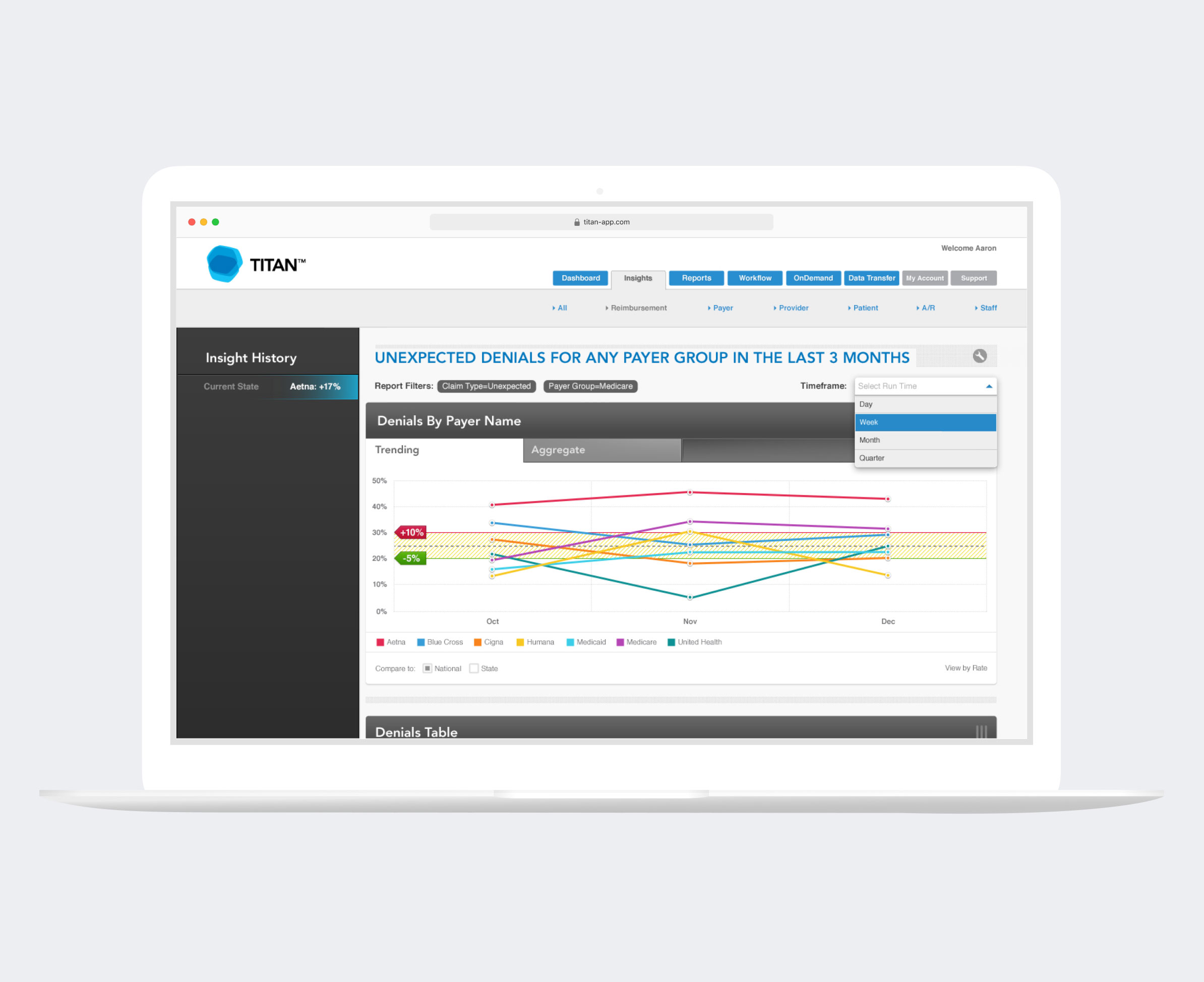
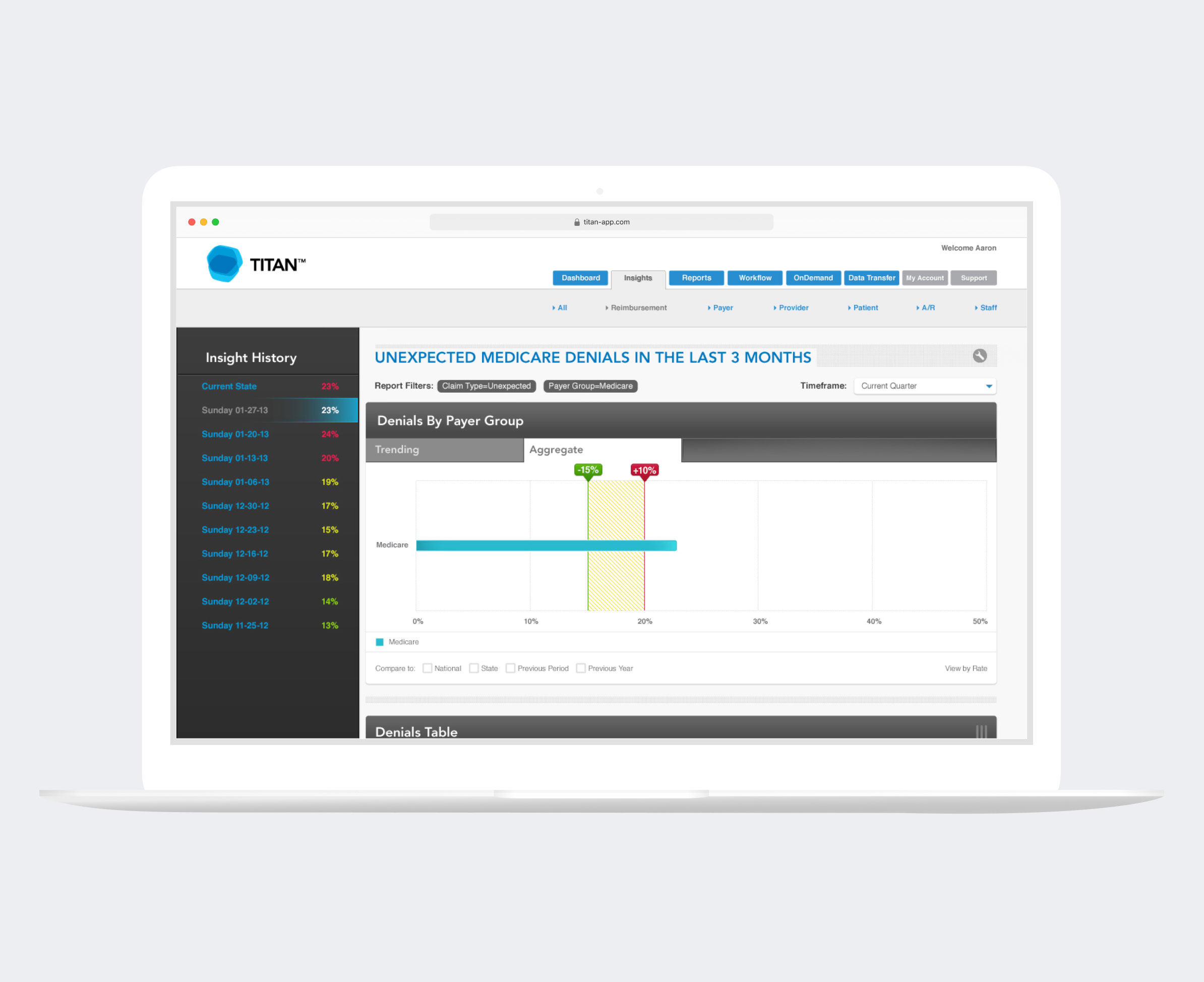
Drilling down from a fully customizable dashboard, TITAN let providers view trend metrics, set targets, and define alerts for various KPIs across multiple departments. Providers could set up insight alerts for proactive monitoring of specific metrics and custom threshold levels for performance.

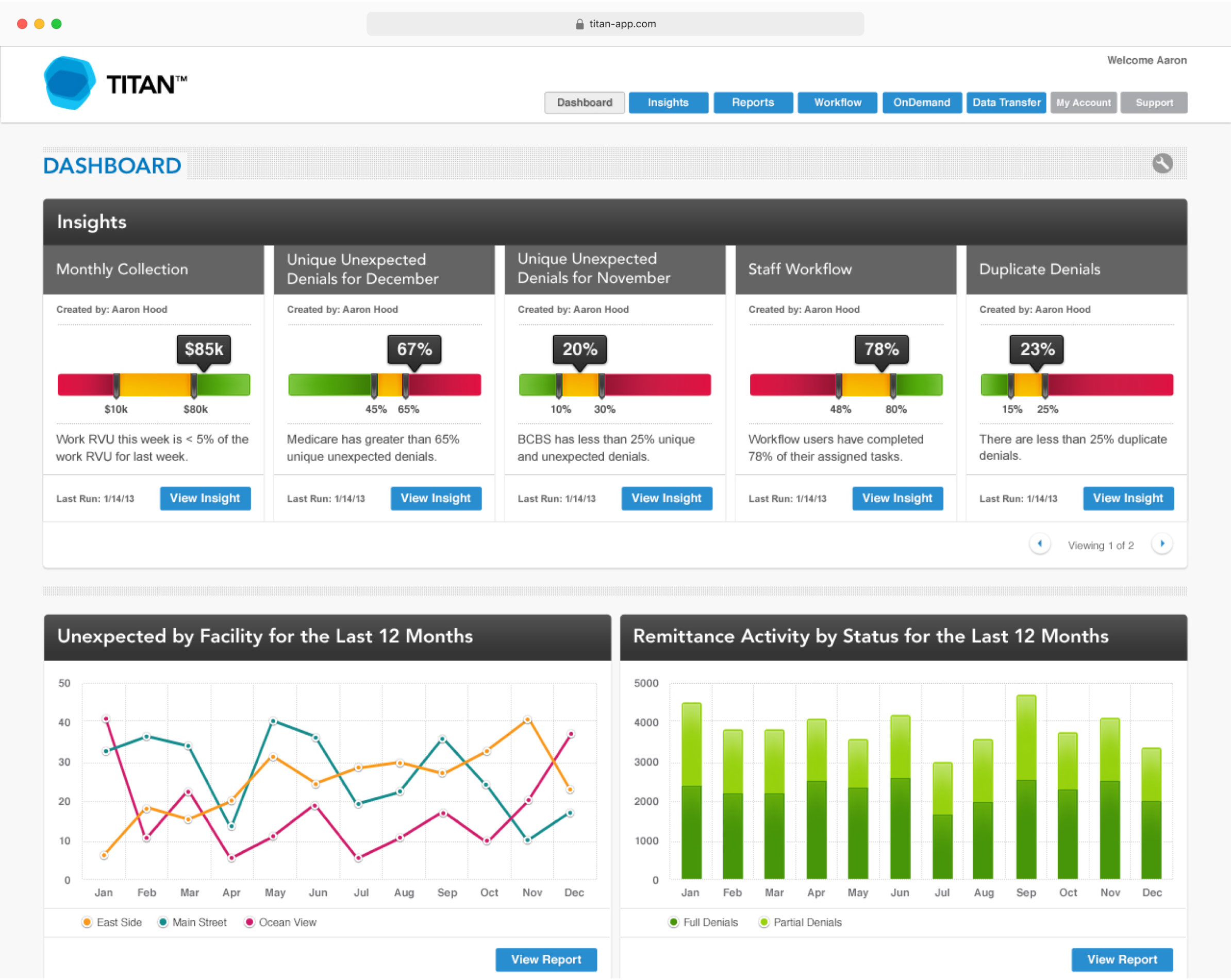
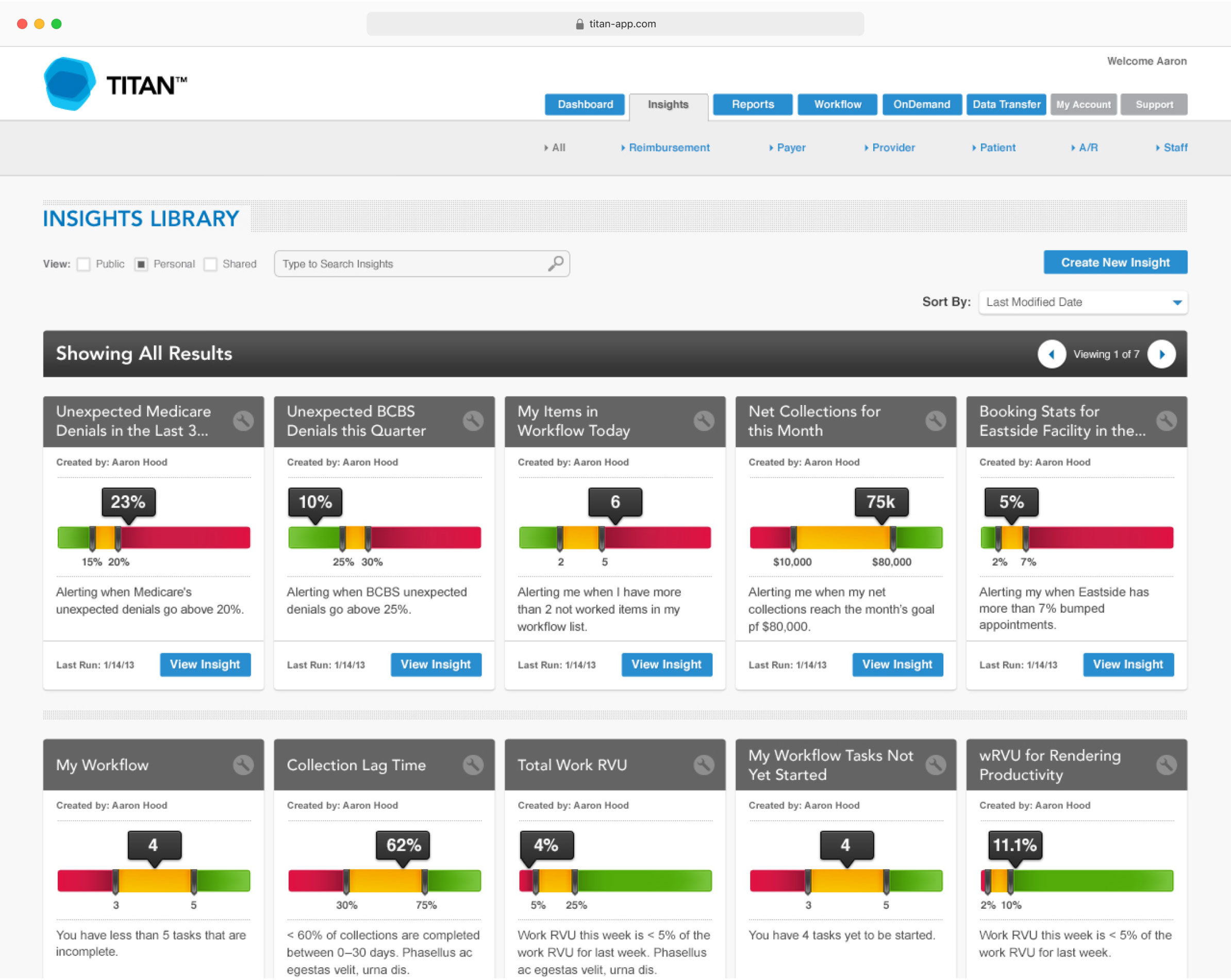
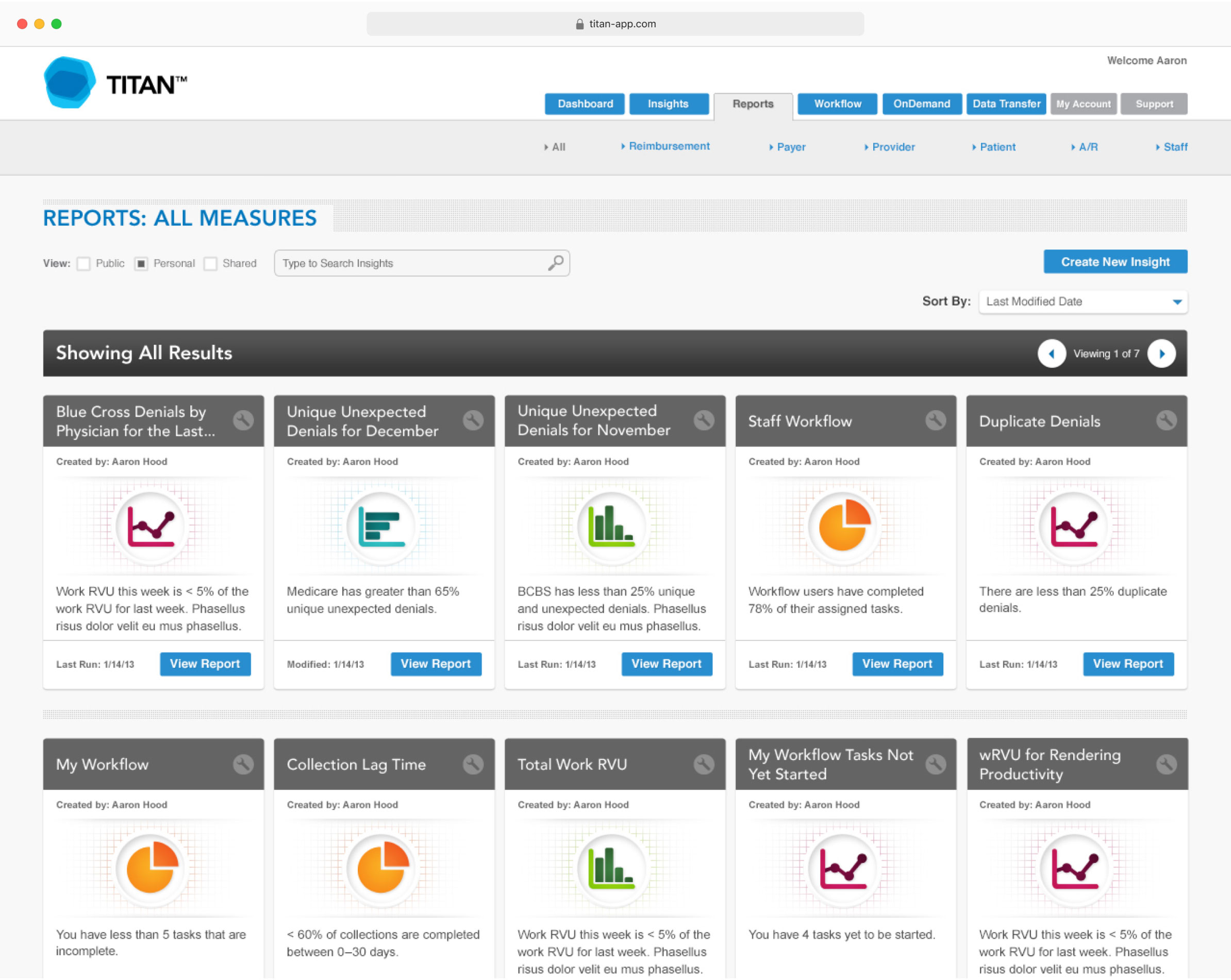
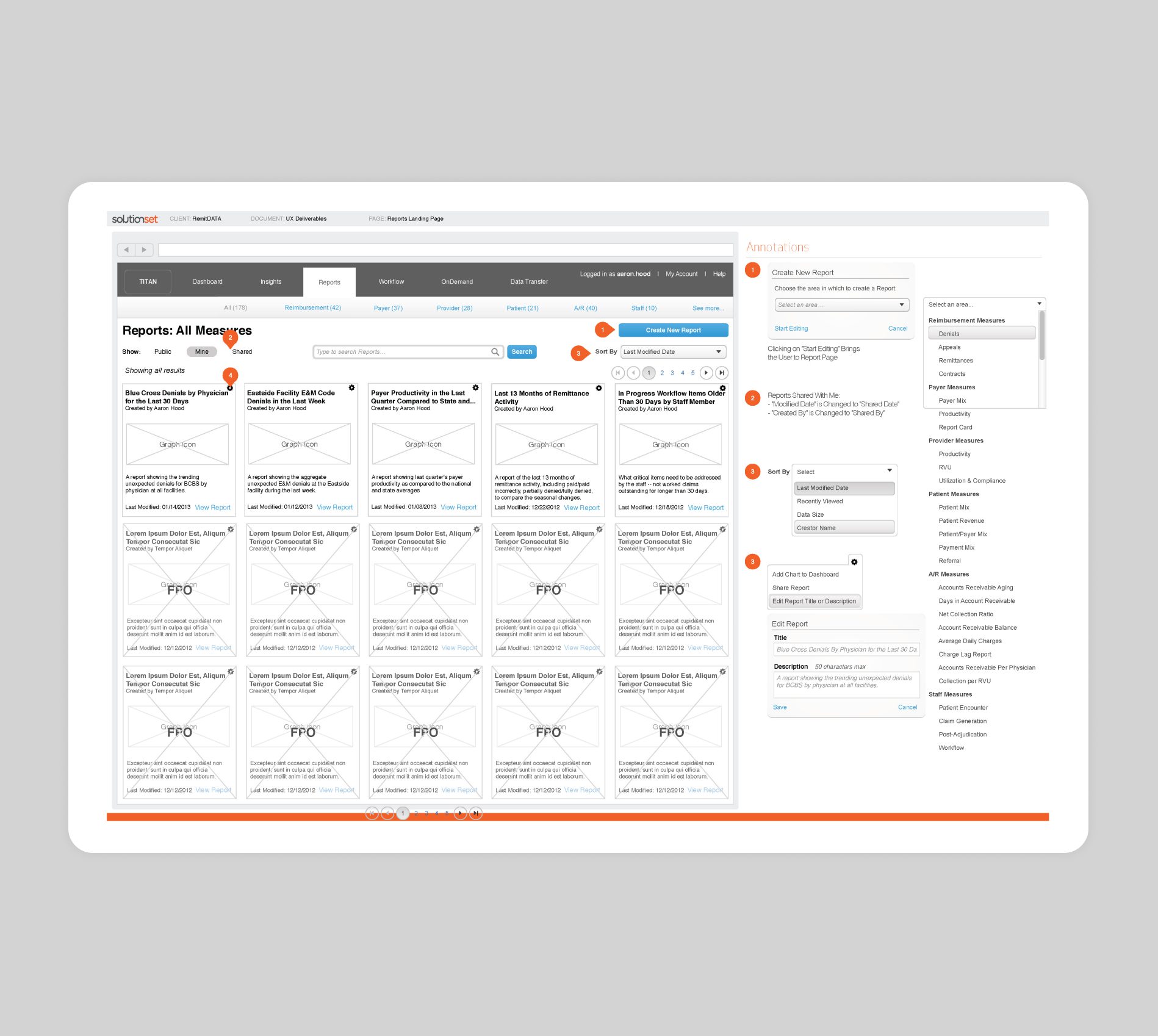
The ability to dissect a variety of metrics for comparison against peers allowed providers to make more strategic business decisions. Providers could quickly understand where to focus their resources to ensure they operate as efficiently as possible to achieve their revenue goals.
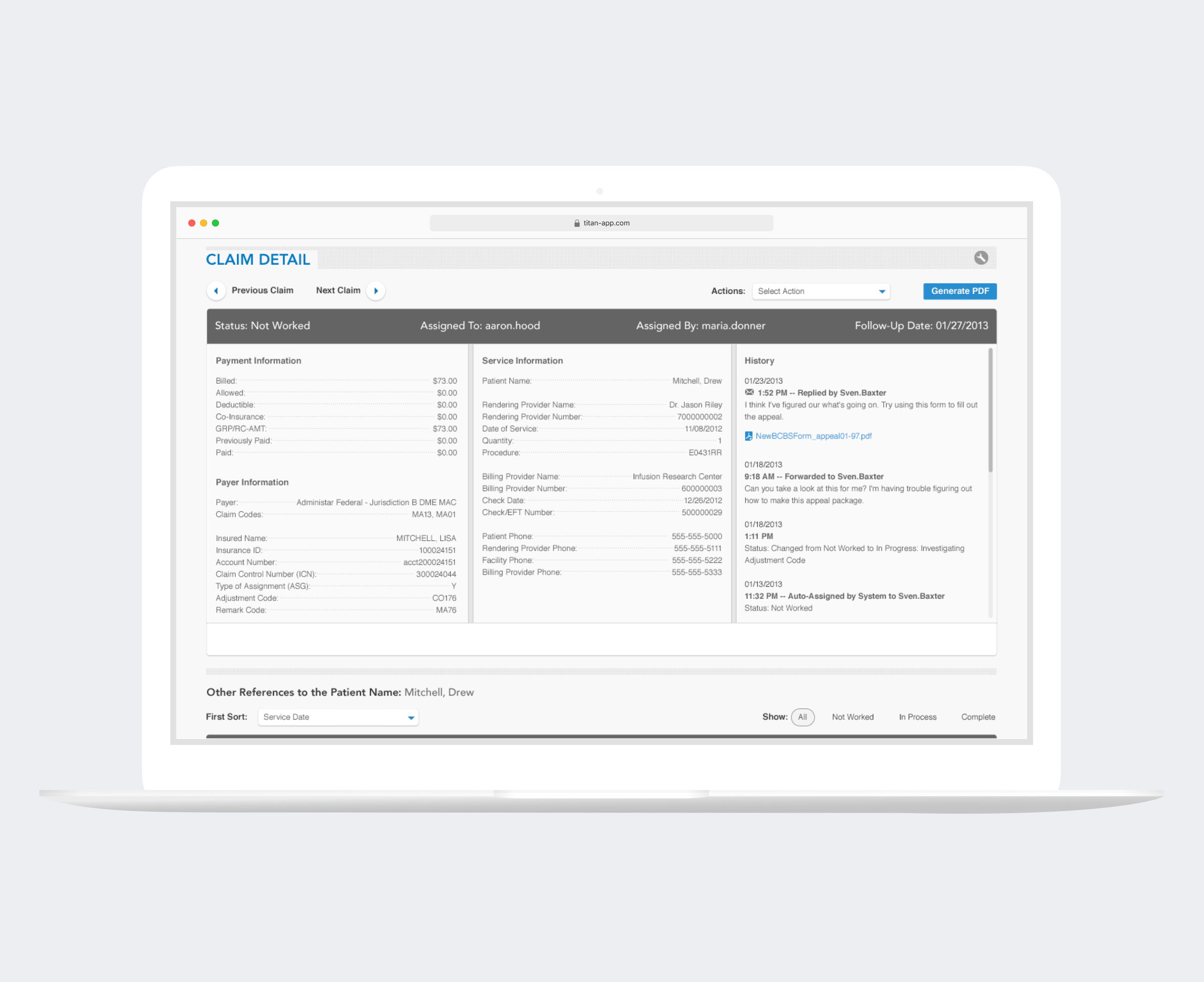
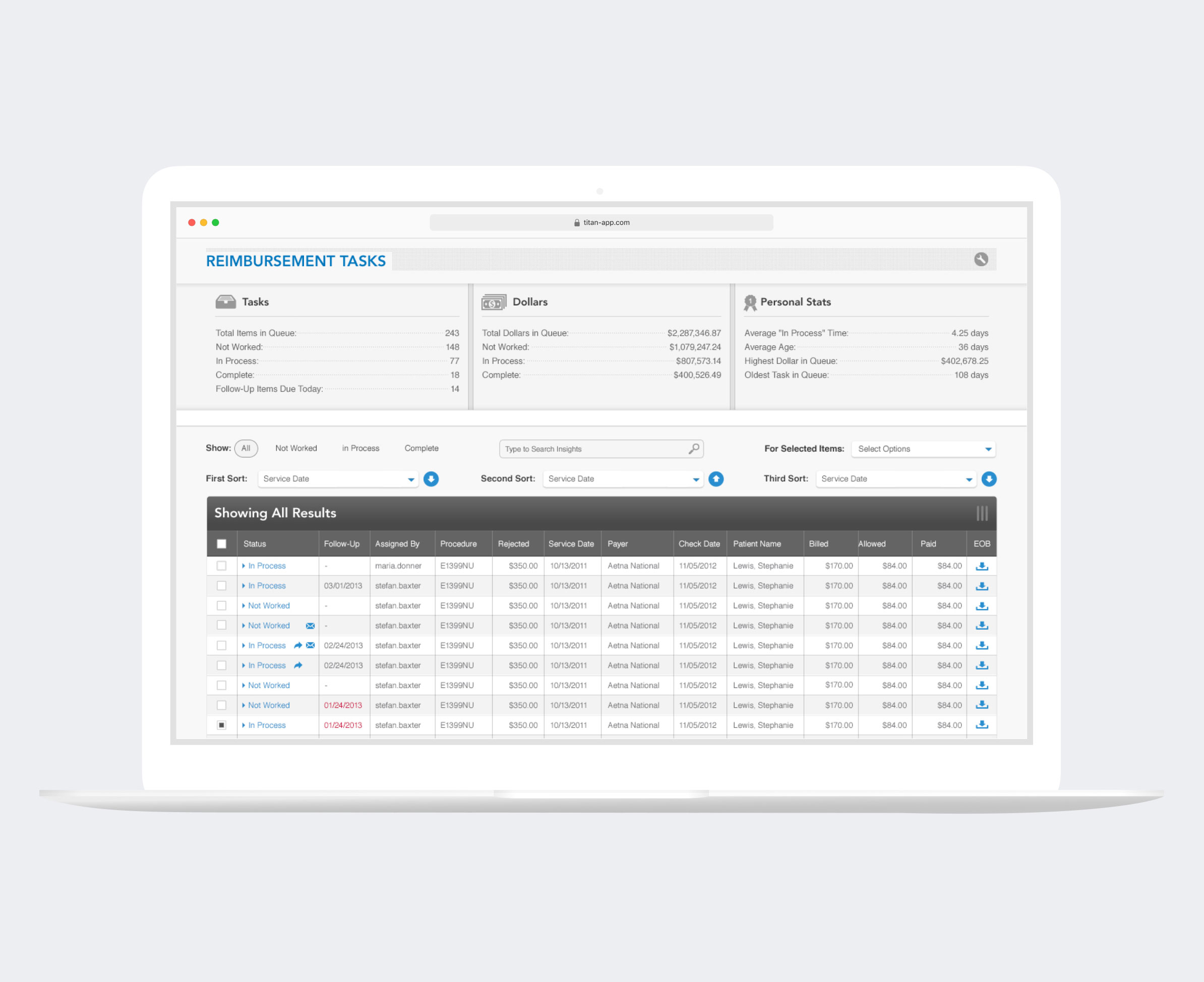
Claim details provided information about each patient, allowing for hyper-detailed insights and clear next steps. Reimbursement tasks could be assigned across an organization, allowing for transparency on who is working on what and the efficiencies and revenue gained as teams complete their to-do lists.
A customizable visual rules-based system allowed a clear view of how a denial type flow is structured and how many claims have been processed using it.